Evidence Based Practice Revolutionizing Care
Ever wonder how healthcare professionals make decisions that impact your well-being? It's not magic, it's method. Increasingly, it's a method rooted in scientific rigor and proven effectiveness: evidence-based practice in care. This approach is shaking up the healthcare landscape, demanding we ditch outdated practices and embrace what truly works.
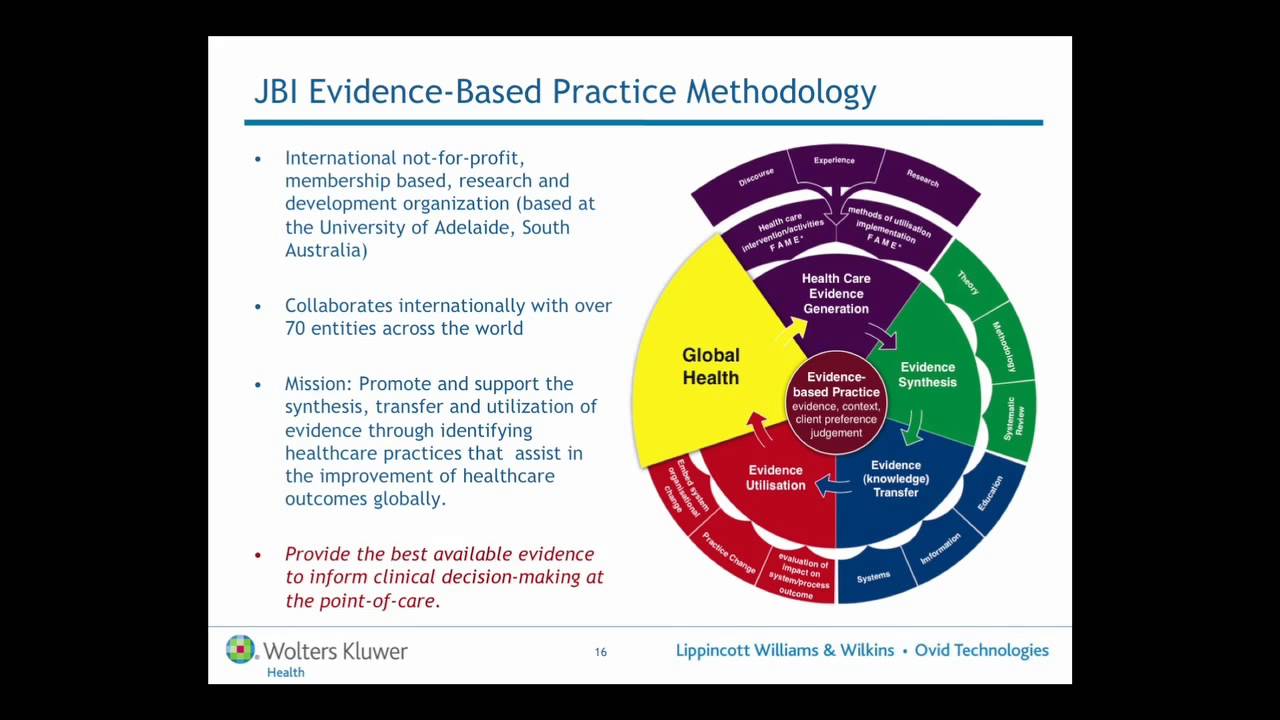
Evidence-based practice (EBP) in care isn't just a trendy buzzword. It's a systematic approach to healthcare delivery that emphasizes utilizing the best available research evidence, combined with clinician expertise and patient values, to make informed decisions about patient care. This means moving away from "we've always done it this way" and towards "what does the research say?"
The roots of evidence-based practice can be traced back to the mid-19th century with the rise of evidence-based medicine. Pioneering figures like Florence Nightingale championed data collection and analysis to improve sanitary conditions and reduce mortality rates. However, the formalization of EBP as we know it today gained momentum in the 1990s, driven by a growing recognition of the variability and sometimes ineffectiveness of traditional care practices.
Implementing EBP in care is crucial for a number of reasons. It leads to better patient outcomes, reduces healthcare costs by eliminating ineffective interventions, and empowers healthcare professionals to make confident, data-driven decisions. However, putting EBP into practice isn't always easy. Challenges include access to research, time constraints, and resistance to change within healthcare systems.
A simple example of EBP in action is the use of hand hygiene protocols to prevent infections. Decades of research demonstrate the effectiveness of handwashing in reducing the spread of germs. EBP translates this research into practical guidelines and training programs for healthcare workers, leading to tangible improvements in patient safety.
One benefit of evidence-based practice is improved patient outcomes. By basing care on the latest scientific evidence, patients are more likely to receive effective treatments and experience better health outcomes. Another benefit is reduced healthcare costs. EBP can help eliminate unnecessary or ineffective interventions, leading to cost savings for both patients and healthcare systems. Lastly, EBP empowers healthcare professionals. By equipping them with the knowledge and skills to critically evaluate research and make informed decisions, EBP enhances professional confidence and job satisfaction.
A practical action plan for implementing EBP involves five steps: 1) Formulate a clinical question, 2) Search for the best available evidence, 3) Critically appraise the evidence, 4) Integrate the evidence with clinical expertise and patient preferences, and 5) Evaluate the effectiveness of the intervention.
Advantages and Disadvantages of Evidence-Based Practice
| Advantages | Disadvantages |
|---|---|
| Improved patient outcomes | Time-consuming to research and implement |
| Reduced healthcare costs | Access to research may be limited |
| Empowered healthcare professionals | Resistance to change from traditional practices |
Best practice examples: 1) Implementing hand hygiene protocols. 2) Using standardized pain assessment tools. 3) Implementing fall prevention programs in hospitals. 4) Promoting breastfeeding for newborns. 5) Utilizing evidence-based guidelines for managing chronic conditions like diabetes.
Real examples: 1) A hospital reduced surgical site infections by implementing evidence-based hand hygiene protocols. 2) A nursing home improved resident mobility by implementing an evidence-based fall prevention program. 3) A clinic improved diabetes management by implementing evidence-based guidelines for patient education and self-care. 4) A pediatrician promoted breastfeeding by providing evidence-based information to new mothers. 5) A hospital reduced readmission rates for heart failure patients by implementing an evidence-based care transition program.
Challenges and solutions: 1) Lack of time - Allocate dedicated time for EBP activities. 2) Lack of access to research - Utilize online databases and libraries. 3) Resistance to change - Engage stakeholders and provide education about EBP. 4) Lack of skills in critical appraisal - Offer training in research methodology and critical appraisal. 5) Difficulty integrating evidence with patient preferences - Develop strong communication and shared decision-making skills.
FAQs: 1) What is EBP? 2) Why is EBP important? 3) How do I implement EBP? 4) Where can I find evidence-based resources? 5) How do I critically appraise research? 6) How do I integrate evidence with patient preferences? 7) How do I evaluate the effectiveness of EBP interventions? 8) What are the challenges of implementing EBP?
Tips and Tricks: Collaborate with colleagues, join professional organizations, attend conferences, subscribe to journals, and utilize online resources to stay up-to-date on the latest evidence.
In conclusion, evidence-based practice in care represents a fundamental shift in how healthcare is delivered. It's about making informed decisions based on the best available scientific evidence, clinical expertise, and patient values. The benefits are undeniable – improved patient outcomes, reduced costs, and empowered healthcare professionals. While challenges exist, embracing EBP is essential for moving healthcare forward. It's time to move beyond tradition and embrace the future of care—a future informed by evidence, driven by data, and focused on achieving the best possible outcomes for every patient. The continued integration of research, clinical expertise, and patient preferences is not just a trend, but a necessary evolution in healthcare, promising improved well-being for all. Become a champion for evidence-based care, and join the movement towards a brighter, healthier future.
Decoding boat hull numbers a deep dive into maritime identification
Unlocking the enigma the true color of chamois
Dominate your bracket unlocking march madness predictions