Humana Gold Plus HMO Claims: Your Guide to Streamlined Healthcare
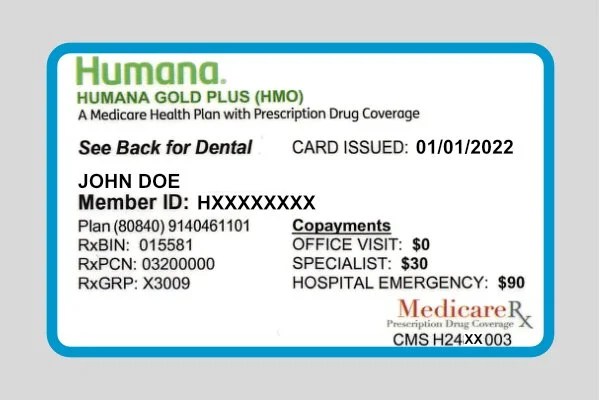
Dealing with health insurance claims can feel like navigating a maze. Where do you send them? What information is required? How long will it take? If you're a Humana Gold Plus HMO member, understanding the ins and outs of the claims process can save you time, money, and frustration. This guide breaks down everything you need to know about Humana Gold Plus HMO claim submissions.
Finding the correct Humana Gold Plus HMO claims address is crucial for timely processing. While a quick online search might yield multiple results, it's essential to ensure you have the most up-to-date information. Humana's website is the best resource for this, offering a dedicated member portal where you can locate the specific mailing address for your plan. This portal often personalizes information based on your individual policy, ensuring accuracy.
Submitting claims effectively is key to receiving reimbursement. While understanding where to send your Humana Gold Plus HMO claims is vital, knowing what to include with your submission is equally important. Typically, you'll need to submit a completed claim form, along with any supporting documentation such as itemized bills and medical records. Organizing these documents and ensuring they are legible can significantly expedite the process.
Why is understanding Humana Gold Plus HMO claims submission so important? Efficient claims processing translates directly to timely reimbursement for your medical expenses. It minimizes the risk of claim denials due to errors or incomplete information. Moreover, a clear understanding of the process empowers you to take control of your healthcare finances and avoid unexpected costs.
Humana, a major player in the health insurance industry, offers a variety of plans tailored to different needs. Humana Gold Plus HMO is designed for those seeking comprehensive coverage within a network of providers. This type of plan emphasizes preventative care and coordinated services. The history of HMOs and their evolution highlights the importance of managed care in providing cost-effective healthcare solutions. One common issue related to HMO claims is the need for pre-authorization for certain services. Understanding these requirements is essential to avoid claim denials. Always check your policy details for specific pre-authorization guidelines.
A common question among Humana Gold Plus HMO members is, "What if my claim is denied?" Humana offers an appeals process for denied claims. It's important to understand the reasons for the denial and follow the outlined appeals procedure carefully. Documentation is crucial during the appeals process, so keep records of all communication and supporting evidence.
One benefit of Humana Gold Plus HMO is the emphasis on preventive care. This can lead to early detection and treatment of health issues, potentially reducing long-term costs. Another advantage is the coordinated care within the HMO network, which streamlines communication between providers and helps ensure a more holistic approach to healthcare.
Advantages and Disadvantages of HMO Plans
| Advantages | Disadvantages |
|---|---|
| Lower premiums and out-of-pocket costs | Limited provider network |
| Emphasis on preventive care | Need for referrals to see specialists |
One best practice for managing Humana Gold Plus HMO claims is to keep meticulous records of all medical expenses, receipts, and correspondence. This organized approach simplifies the claims process and ensures you have the necessary documentation if a claim is questioned or denied.
Frequently Asked Questions:
1. Where can I find the Humana Gold Plus HMO claims address? Answer: Check the Humana member portal for the most up-to-date address specific to your plan.
2. What information do I need to include with my claim? Answer: A completed claim form, itemized bills, and relevant medical records.
3. How long does it take to process a claim? Answer: Processing times can vary, but typically it takes a few weeks.
4. What if my claim is denied? Answer: Follow Humana's appeals process, providing supporting documentation.
5. What are the benefits of preventive care? Answer: Early detection and treatment, potentially reducing long-term costs.
6. Do I need referrals to see specialists? Answer: Yes, HMOs generally require referrals.
7. How can I check the status of my claim? Answer: Log in to the Humana member portal or contact customer service.
8. What are some common reasons for claim denials? Answer: Incomplete information, lack of pre-authorization, or services not covered by the plan.
One tip for managing your claims is to sign up for electronic explanations of benefits (EOBs). This allows you to access your claim information online quickly and easily.
In conclusion, navigating Humana Gold Plus HMO claims requires understanding the process, staying organized, and utilizing available resources. By being proactive and informed, you can ensure timely reimbursement and effectively manage your healthcare expenses. Taking advantage of the Humana member portal, keeping detailed records, and understanding the appeals process are key steps in successfully navigating the claims process. Remember that clear communication with Humana and your healthcare providers is essential for a smooth and hassle-free experience. By taking control of your healthcare finances and utilizing the resources available, you can minimize stress and maximize the benefits of your Humana Gold Plus HMO plan. This empowers you to focus on what matters most: your health and well-being.
Outdoor plug problems why your power keeps tripping
Ditch the dye embrace gorgeous grey with natural henna
Unlocking the power of r your guide to genshin impacts r starting characters